Fluoride in Water, Fluoride Toothpaste, Fluoride Dangers...
Fluoride: Is it Good or is it Bad for us? Should I use it or avoid it? If you Google “fluoride good” you will get about 21 million results. If you...
6 min read
Dr. Joanne Baldos and Dr. Adam Szymczak : Sep 28, 2022 4:30:00 AM

There is a link between oral health and overall health!
For example, COVID-19 patients with gum disease are:
COVID has lead many people to loose many teeth. However, COVID does not directly cause tooth loss. To understand how COVID leads to tooth loss, one must understand the interconnectedness of human health:

There has been a tremendous amount of reporting regarding COVID. However, there has been a lack of focus on information regarding overall well-being. Two critical areas not discussed often enough are mental health and oral health, which are essential to overall well-being.
The COVID pandemic has had a devastating effect on the world. The virus has killed over 6.5 million people and caused widespread disruption to everyone's lives:
As people grapple with these health, social and economic impacts, mental health has been widely affected. Many people have become more anxious, but COVID-19 has sparked or amplified much more severe mental health problems for some. Many people have reported psychological distress and depression, anxiety, or post-traumatic stress symptoms.
We have worked with people face-to-face throughout the pandemic. We have seen firsthand, heartbreakingly, the effects of COVID on mental health, affecting oral health and overall health.
An area that has received even less attention is the effect of COVID on oral health, and yet the impact of COVID on oral health has been profound. It is estimated that over 2 billion people worldwide are at risk for dental problems due to COVID.
To understand the effect of COVID on oral health, it's of value to review the link between oral health and overall well-being.

nature.com, a respected medical publication, explains that tooth decay and gum disease are the most common human diseases with debilitating effects:
"In 1990, oral diseases, principally dental caries, and periodontitis were the most common human diseases when 354 causes of disease and injury were analyzed across 195 countries by the Global Burden of Diseases study. This alarming statistic remained unchanged in 2017, with 3.47 billion cases worldwide. Indeed, periodontal disease and caries were ranked 14th and 16th in their contribution to years lost to disability in women and men, respectively, is responsible for more years lost to disability than any other human disease."
The Surgeon General’s Report on Oral Health has made it clear that oral health is part of overall health and well-being:

According to CDC: "oral health means much more than healthy teeth; it is integral to the general health and well-being." The mouth reflects general health and well-being. Oral diseases and conditions are associated with other health problems.
In particular, periodontitis has been independently associated with over 57 human diseases, the most important of which are:
The mechanisms through which oral health is connected to other diseases within the body are complex. These include bacteremia and the associated systemic inflammatory sequelae, including elevated C-reactive protein and oxidative stress.

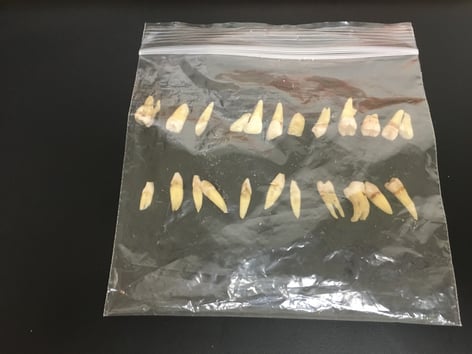
Unfortunately, this is one of many patients whose oral health was destroyed by COVID. Instead of discussing only this patient's COVID journey, it is more constructive to discuss the collective experience of all such patients.
COVID does not directly cause loss of teeth. COVID causes tooth loss indirectly by increasing the chance and progression of gum disease (periodontal disease) and tooth decay (cavities).
The most significant reason people have unnecessarily lost teeth during the pandemic is delaying going to the dentist. Early in the pandemic, it seemed to make sense; people were told that we should avoid face-to-face interactions and wear masks, neither of which is possible at a dental visit. We now know that a dental office is the safest place during a pandemic. There have been COVID outbreaks in hospitals, grocery stores, gyms, long-term care homes, schools, factories, warehouses, and hotels BUT not one outbreak at the dentist! Due to the constant media barrage of fear-based information, many people were gripped by severe anxiety and depression. They could not even leave their house, let alone go to the dentist. The reason why avoiding the dentist leads to loss of teeth is explained by the next point.
Pain in the body alerts us to something being wrong. However, the opposite, "lack of pain," does not mean everything is well. For example, an artery in the heart has to be over 50% blocked before the body will let you know by causing chest pain (angina pectoris). For slow-developing conditions (chronic conditions), pain is a late warning sign within the body. By the time there is a toothache, the tooth is often not savable or needs extensive treatment, such as a root canal. Tooth decay and gum disease progress in very predictable ways; the earlier these diseases are discovered, the more predictable and less costly the process of halting the disease process. This is, in part, why regular visits to the dentist prevent tooth loss.
Saliva prevents tooth decay and gum disease:
COVID directly causes decreased salivary flow. Furthermore, wearing a mask encourages mouth breathing which causes the mouth to dry up. Less saliva means more cavities and more gum disease.
Some people took matters into their own hands regarding dry mouth; they used lozenges to stimulate salivary flow. The consequences have been disastrous: rampant tooth decay!
Decreased saliva means a decreased defense against tooth decay
+ sugar in the lozenges feeds the decay-causing bacteria
= rampant tooth decay
Psychological stress and symptoms of depression and anxiety disorders lead people to decrease their oral hygiene regimens. Bacterial overgrowth in the mouth leads to tooth decay and gum disease.
Stress, anxiety, and depression decrease salivary flow, reducing the protective effect of saliva.
The 30 years of work in the field of psychoneuroimmunology have convincingly established that chronic stressful experiences alter the immune response, leading to other health problems. Stress increases the chance of and worsens periodontal disease.
A sedentary lifestyle during the pandemic (nowhere to go, nothing to do) combined with easy access to unhealthy food within reach as people worked from home led to 48% of people gaining weight. People who are overweight are more likely to have periodontitis. Obesity is characterized by a chronic subclinical inflammation that exacerbates other chronic inflammatory disorders like periodontitis.
Foods containing sugar feed the cavity-causing bacteria directly, which in turn causes cavities.
Some people grind and/or clench their teeth when sleeping. Teeth grinding is related to stress and has been more common and intense during the pandemic.
Bruxism will make existing gum disease worse. The force from clenching and grinding damages the tissues that hold the teeth in place, deepening periodontal pockets and loosening teeth. This makes the gums more vulnerable to infection, and the disease spreads faster than usual.
Grinding leads to cracked teeth. The average maximum bite force in the first molar area is 200 pounds, which is what our teeth were designed to hold up to. A person that grinds teeth exercises their jaw muscles every night; as such, they can generate over 1000 pounds of force per square inch. These kinds of forces lead to tooth loss.
A COMBINATION OF THE FACTORS ABOVE CREATES A PERFECT STORM AND RESULTS IN PROFOUND TOOTH LOSS. We hope that this information will help others prevent the same fate. It is heartbreaking for us as dentists to see patients whose best option is to remove all their teeth.
In the best interest of your health and well-being,
Dr. Joanne Baldos and Dr. Adam Szymczak
P.S. People that you know will benefit from this information. Please share this information with your family, friends, and colleagues. (the best way to share is to email people with the link to this page OR clicking the social sharing links at the top of this page)

Fluoride: Is it Good or is it Bad for us? Should I use it or avoid it? If you Google “fluoride good” you will get about 21 million results. If you...

There are only two body parts that are DESIGNED to be lost: the umbilical cord baby teeth Some people MISTAKENLY believe that because baby teeth...

1) No Need to Floss Anymore, Replace Your Floss with a Rinse! OR 2) Brush and Floss to Keep Dental Problems Away